Over the years, I have followed several radiation safety courses in a variety of countries. Last week, it was NIMS’ turn to train me. As this was given in Japanese (a language I can only half follow), I decided to write my own section on radiation safety instead (for future inclusion in the book). This will draw on personal experience, things I remember from previous trainings and google’d knowledge, but I am fairly sure much of this is correct. Nevertheless, it is only in draft stage, and will still require an expert check, so use this at your own discretion.
[First and foremost: don’t be stupid, be a smartie, and use common sense in the lab. If you are pressured into doing unsafe things, consider whether or not it is safer to proverbially whack your tormentor with a clue-by-four (instead of putting your own life on the line). “Nobody has been injured yet” is not a good excuse for unsafe practices.]
Introduction:

more examples: http://www.biij.org/2007/2/e22/
While working with ionizing radiation automatically elevates your status in social circles to the “cool” level (as does working with lasers, explosives and underwater robots), we should not forget that we are working with an invisible source of potential harm. Radiation sources (informally known as “ray guns” to those born in the fourties) are increasingly focused, of higher intensity, and more compact than their predecessors. This means that it is now easier than ever to walk away with (at minimum) some radiation burns or not-so-cool skin transplants (Figure 0, more information on radiation burns here, Some more (graphic) examples of radiation burns can be found in this paper).
For those who have X-ray instruments, be they in-house developed or commercially acquired, basic knowledge on radiation safety is quite handy. I have experienced failures of both types of instruments, and I have been exposed to light doses of radiation in both cases. Fortunately, no injuries followed, but I will discuss both cases later on as examples.
In addition to simple instrumental failures, there are times when, due to time constraints, curiosity or frugality, you need to align your instrument manually. For many lab instruments, alignment procedures require working with open X-ray sources to some degree.
The purpose of this section is to provide a little guidance on radiation safety, and what should be done in case of accidental exposure. This section will discuss radiation safety for typical electronically driven laboratory X-ray sources only, not safety for (handling) radioactive material or (working with) neutron sources.
Procedure:
To be frank, the current administrative environment is counterproductive to handling the latter aspect correctly: at the moment it is indicated that accident reporting in particular is to be “punished” by a deluge of paperwork and future restrictions. This atmosphere actively discourages people from reporting, endangering their own health in the process.
When done right, the following should happen in case of an accident:
- You accidentally expose yourself (expletives are uttered at this point)
- You hit the emergency generator shutoff.
- You tell your boss or your colleague. They will then take you to the correct person. N.B.: by no means should you feel ANY barrier to reporting.
- The correct person will, at this point, take over the case and handle the paperwork (very important, your responsibility ends here!). You sit back, relax and follow his or her instructions.
- You will be guided through the steps to estimate your exposed dose on the affected body parts.
- Based on this estimation, any required action can be undertaken to minimize health hazards to you (f.ex. monitoring of affected areas, body condition, or first aid).
- After this, reasonable modifications can be done to the instrumentation or procedure to prevent similar incidents without overly complicating the operation thereof.
The key points here are that your exposure and health effects are assessed, and any preventative measures taken accordingly (blood and/or skin tests, etc.). This way, effects can be minimized. Don’t wait for the gangrene to kick in! Accidents are nearly inevitable in the laboratory, and should be properly handled and learned from.
So how can you get exposed? What about the safety interlock system in place? For this, I can tell you my two personal stories. Feel free to add your own in the comment section below.
Examples of accidents:
The first was long ago in a small laboratory. After months of research, we were trying an odd experiment. It was the end of a long and hectic day. Before the end, though, I wanted to interrupt and adjust the sample so the measurement could be done overnight.
This was a commercial instrument, so safety interlocks were supposed to be in place. When I forgot to close the shutter, opened the instrument and adjusted my sample, I exposed my finger to the X-ray beam for a second or so.
What followed was textbook handling: my colleague called the correct people, handled the paperwork and we estimated my exposure with the help of a medical expert on radiation exposure. Monitoring of the affected finger showed no visible damage.
So how did this happen? It turns out that the safety interlock had been properly connected, just to the wrong beam port (X-ray tubes typically have four ports). Interrupting the safety circuit, therefore, did nothing as that beam port was not open. Secondly, I didn’t pay attention to close the shutter on that event, unlike the prior months.
Second case: A few years later, we had an interesting problem with a Rigaku rotating anode generator (I dislike this particular brand of generators for a variety of reasons). For those who know this type of generator, older shutters tend to get corroded and get sticky (which has led more than one researcher to bang on the shutter housing with a hammer).
In this case, the shutter had been closed, and reported it *was* closed (the small indicator light was off). Fortunately, after opening the sample chamber but just before unscrewing the sample holder, we noticed the detector was still counting! Apparently, the shutter was having issues and got stuck on the way down.
Months later, with the arrival of my dosimeter (film badge) results, we noticed a slight elevation in exposure, likely due to this incident (open sample environment, air scattering of the beam).
So those are two examples of accidental exposure. They serve as an example that even with ostensibly “safe” instrumentation, exposures still happen. For this reason, I oppose the current (minor cost saving) efforts to reduce dosimeter usage for casual workers. When an accident occurs, noticed or unnoticed, it can provide an approximate record of exposure.
Measuring radiation exposure:
Measurements matter, in this case they can help define problems. So what measures are important in radiation safety (I will stick to proper SI units here)?
- The Becquerel (Bq) is typically the first measure you hear about during radiation safety lectures. It is the measure for radioactivity, denoting the number of nuclear decays per second. To know how much, and what radiation is emitted, you need to add information on the composition of the material. This is not very useful in our case, as we have ionizing radiation emitted from our sources from Brehmsstrahlung and characteristic emission lines.
- Gray (Gy): This is more useful for us, it is the measure of energy absorbed by matter, in J/kg (
). Since we know the energy spectrum (and flux) of our X-ray generators, both before and after monochromatization, we can calculate the energy and flux of the radiation at the point of impact. Using this, we can estimate the absorption volume in human tissue. There are only three shades of Gray typically used: absorbed dose, specific (imparted) energy and kerma.
- Sievert (Sv): This is the one most people are familiar with, in particular after the neverending TEPCO fuck–ups in Fukushima (leading to awesome public radiation monitoring projects). It is an approximate measure of health effects (for low radiation levels), indicating stochastic health risk. It is the probability of cancer induction and genetic damage. One Sievert is equivalent to a 5.5% increase in chance of developing cancer. It is typically calculated based on Gray, multiplied with a weighting factor for uniform body exposure, or multiple weighting factors for localised exposure to organs.
This last unit is quite fun to calculate with. The equivalency means that we can estimate equivalent doses for activities unrelated to radiation.
For example, the average rate for cancer is 0.2% of the population per year. This is equivalent to receiving a dose of 36 mSv per year. Regular exercise reduces cancer risk by about 40%, so that would be -15 mSv per year.
To put this in perspective, normal male smokers’ lifetime risk of lung cancer is 15.9 %. This would be equivalent to a total received dose of 2.9 Sv of radiation (9.5%, 1.7 Sv for women). (Other ways of improving health also include standing up at your desk, leaving the office and never coming back.)

Anyway, what are the limits for radiation workers? Typically, trained staff is allowed to receive a maximum of 50 mSv per year, to a maximum of 100 mSv per five years (most countries, as does Japan, subscribe to these limits). The general public is allowed to only receive 1 mSv of radiation exposure per year. To get a better feel on Sieverts, XKCD has a handy diagram (Figure 1).
Notes for X-ray generators:

X-ray generators have some peculiarities that are good to be aware of. The first is that the energy of X-ray photons it emits is mostly decided by the target material. The lower the energy, the more any accidental exposure will be concentrated on the skin (but underlying tissue will be undamaged), leading to burn wounds similar to sun burns. With high-energy sources, the skin will be less damaged, but underlying tissue will also be affected.
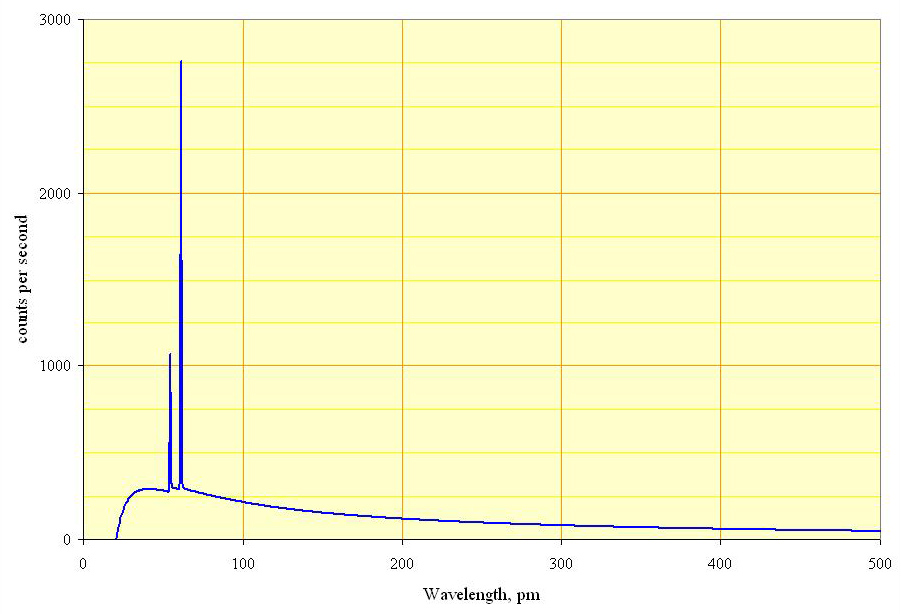
Secondly, unmonochromated beams from laboratory X-ray sources will also contain higher energy bremsstrahlung (up to approximately the acceleration voltage of the source, Figure 2). An unmonochromated beam is therefore much more dangerous than a monochromated beam: not only does it carry a higher flux of photons, it also contains a wide spectrum of radiation, damaging both the skin and the underlying tissue.
Thirdly, normal “radiation safety” advice indicates that a good safety measure is to increase the distance to the source. Unfortunately, most X-ray sources are focused quite well, negating this effect somewhat. Distance will, however, increase absorption by air, leaving only the high-energy radiation for you to enjoy.
Lastly, scattering of radiation by air means that the environment around an unprotected beam will also be a zone with increased levels of ionizing radiation. Be careful in and around sources.
I hope this has been somewhat helpful to you to get an idea about radiation safety. Take the time to learn a little about it, and you will know what to do when something happens.

Leave a Reply